(This is Part 25 of Dr. Pagtakhan’s column Medisina at Politika.)
[Editor’s Note: In February 2020, CFNet started publishing Dr. Rey Pagtakhan’s column, Medisina at Politika, on COVID-19. Now on Part 25 of his running commentary, Dr. Pagtakhan’s twice a month column has kept the Filipino community and other CFNet readers continually informed about 1)the pandemic and its impact, 2)the scientific advances on drugs and vaccines, and 3)the effectiveness of public health responses, including mass vaccination as a necessary path to individual protection and population or ‘herd’ immunity.]
Could Canada vaccinate all Canadians against COVID-19 by the end of this year? By December 31, 2021 New Year’s Eve?
The path to end the pandemic is neither easy nor straight. It is not without unforeseen obstacles to hurdle and challenges to confront. That makes it all the more evident that we need to put the best of our minds and the humility of our hearts to trust each other when questions are asked and answers are given; when we search for solutions to solve problems that emerge during our public health journey. We shall walk hand-in-hand with collaborative and coordinated approaches, not mixed messages and steps from governments and public health officials, as we continue to travel the necessary path – uneven as it may be – to end the pandemic for our common good and realize our year-long collective longing for normalcy of life and living.
Magnitude of Disease and Deaths, Globally and in Canada
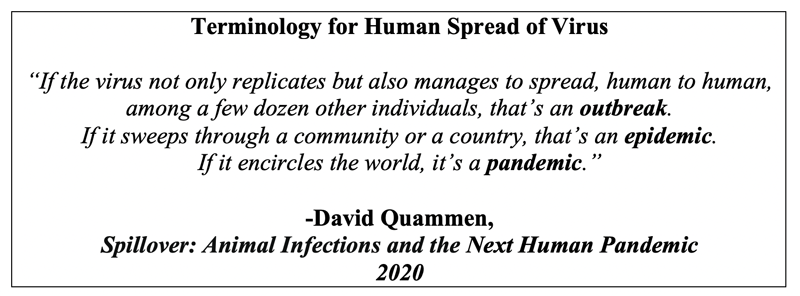
It has been a little over a year since Canada and the world heard on January 30, 2020 that the emerging COVID-19 due to SARSCoV-2, then without these medico-scientific names yet, had been declared by the U.N. health agency – the World Health Organization (W.H.O.) – as a “public health emergency of international concern.” Starting in December 2019 as a cluster of undiagnosed pneumonia in Wuhan, China, and promptly spreading throughout the country and beyond its national borders the following month, the pandemic has since sickened over 108 million and claimed the lives of nearly two-and-a-half million citizens worldwide, including over 820,000 and 20,000 Canadians stricken ill and deceased, respectively (see Table below).'
USA, which has remained the epicenter of the pandemic and appears headed for control under the new Biden presidential leadership, still has nearly 27.5 million cases and deaths trending to half a million. President Joe Biden has made control of this public health misery top of his agenda since his inauguration on the 20th ultimo, and has appointed Dr. Anthony Fauci, the world’s acknowledged pandemic expert, his Chief Medical Adviser and Delegate to the W.H.O., which U.S. has re-joined. The latter move also augurs well for the global aspect of COVID-19 vaccination – a necessity in light of global interconnectedness and travel – were all countries to realize a return to normalcy.
Adverse Events from Immunization Reports
As we collectively champion the need for vaccination, let me share a brief summary of the reports from the Canadian Adverse Events Following Immunization Surveillance System of Public Health Agency of Canada and the Canada Vigilance Program of Health Canada:
- Doses of Pfizer-BioNTech and Moderna distributed = 928,200and 517,700, respectively;
- Total adverse event reports up to February 5, 2021 = 651;
> These represent 651people who reported one or more adverse events;
> Total adverse events = 1,568;
> Majority are mild to moderate (as described in an earlier issue of my Commentary);
> Serious adverse event reports = 99 of the 651;
> 9.5 reports per 100,000 doses administered;
> Occurrence of anaphylaxis was rare;
> No death due to vaccination was seen;
> No vaccine safety issue has been identified.
Global Vaccination Campaign
Said the U.N. World Health Organization recently: “In the COVID-19 vaccine race, we either win together or lose together.”
Indeed, global vaccination against COVID-19 is the universal public health goal, although we acknowledge manufacturing, accessing, delivering and injecting billions of vaccine shots into the arms of billions of people on planet Earth will be a herculean logistical challenge. Yet we all agree it shall be done. This should be the re-assuring message were the world to realize their common medical aspiration.
Fortunately, the race to end the pandemic with vaccination has been enabled to start in December 2020 when two mRNA vaccines – Pfizer/BioNTech and Moderna – received emergency use approvals in the United Kingdom, USA and Canada. [China and Russia have had their own approaches to vaccinating their people even before the data on the results of their vaccine clinical trials were available to the scientific world.] It soon became apparent to European and North American countries and to the other countries of the world that they would experience unequal access to vaccines – until now some have not had any single vial of the COVID-19 vaccine – while others who have had access have experienced, nonetheless, varied logistical problems due to issues related to planning, physical and human resources; manufacturing, supply, storage facilities, and distribution of vaccines; communication, access to and by vaccine candidates, and political leadership.
Global Vaccination - 168M+ Vaccine Shots
The Bloomberg COVID-19 Vaccine Tracker Project reported recently on the following:
- As of February 10th, Israel and the United Arab Emirates have vaccinated more than two-thirds (69% or 68.5 doses injected for every 100 Israeli citizens) and nearly one-half (47%) of their populations, respectively.
- While the United Kingdom and U.S. have vaccinated a fifth (20%) and less than this (15%) of their residents, respectively, the other countries are much lower (under 4% on average), with Canada at 2.52%.
- Globally as of February 12th, over 168 million COVID-19 vaccine shots had been given across 77 countries which have limited access to 7 vaccine brands. Nine more most promising vaccines in development are being followed closely.
- The latest global vaccination rate is 5,902,851 doses daily on average. At this rate, it will take about 5.3 years to vaccinate 75%of the world’s population with a two-dose vaccine.
- Nearly a third of the global vaccines administered – 50.1 million doses– were in the U.S.A.
- With the U.S. population at 331 million, it means about 15.2 vaccine doses have been administered for every 100 Americans and nearly three-fourths (73%) of the shots delivered had been injected into the arms.
While the U.S. has been the pandemic epicenter until now and, understandably, needs that much assured supplies of their domestically produced vaccines, we also take heed of the message from the U.N. Health Agency. In a joint statement from UNICEF Executive Director Henrietta Fore and WHO Director General Dr. Tedros Ghebreyesus, the following message was issued on February 10th:
- UNICEF and WHO call on leaders to look beyond their borders and employ a vaccine strategy that can actually end the pandemic and limit variants.
- Of the 128 million vaccine doses administered so far, more than three quarters of those vaccinations are in just 10 countries that account for 60% of global Gross Domestic Product.
- Almost 130 countries, with 2.5 billion people, are yet to administer a single dose.
- This self-defeating strategy will cost lives and livelihoods, give the virus further opportunity to mutate and evade vaccines, and will undermine a global economic recovery.
- To ensure that vaccine rollouts begin in all countries in the first 100 days of 2021, it is imperative that:
a. Vaccine manufacturers allocate the limited vaccine supply equitably; step up and maximize production; and transfer technology to other manufacturers who can help scale the global supply.
b. Governments that have vaccinated their own health workers and populations at highest risk of severe disease share vaccines through COVAX so other countries can do the same.
Indeed, global leadership is needed to increase vaccine production and attain equitable access to vaccines. Unfortunately, two global powers – China and Russia and, until recently, the U.S. which has since re-joined the WHO following the inauguration of the new U.S. President last month - have apparently declined to support the global effort. Many poor countries around the world stand to suffer. Through COVAX – COVID-19 Vaccines Global Access – Facility, poverty-stricken countries would have a better chance of access to vaccines and their deployment and administration.
What are some of the adverse implications when developed countries fail to heed the need for vaccines by underdeveloped nations? Not only illness and deaths nor ongoing financial hardships from lockdowns, but also increased chances for emergence of more lethal and transmissible virus variants that are vaccine resistant. Their circulation around the world would just lead to vicious pandemic cycles and their complications.
The collateral harms to children – lost schooling, more child laborers, more child brides, increased gender inequality, greater hunger, shorter lives – cannot be excused.
We know that even Canada had its recent struggle with earlier promised supply from foreign firms. The decision to build one or more than one vaccine manufacturing plant is overdue.
Overdue as well is the strategy and commitment on the part of well developed countries to help enable vaccine producers to output more for other countries to timely share, including “openly sharing vaccine manufacturing technology, intellectual property, and know-how through the WHO COVID-19 Technology Access Pool, temporarily waiving intellectual property barriers, and expanding voluntary contracting between manufacturers and enabling to help build additional manufacturing bases—especially in Africa, Asia, and Latin America—which will be essential to meeting ongoing demand for COVID-19 booster shots and future vaccines.”
These are necessities that when fulfilled would also make poor countries less dependent on donations and, thereby, help attain genuine health equality and global health and security.
In a recently released poll survey, it is interesting to note that two-thirds of Britons support the joint call from the UNICEF and the W.H.O.
Where is Canada in Its Mass Vaccination Drive?
Can Canada vaccinate all her residents against COVID-19 by December 31, 2021?
The Table below illustrates the proportion of Canadians, across10 provinces and 3 territories, who have been vaccinated with at least one dose of the two-dose vaccine regimen.
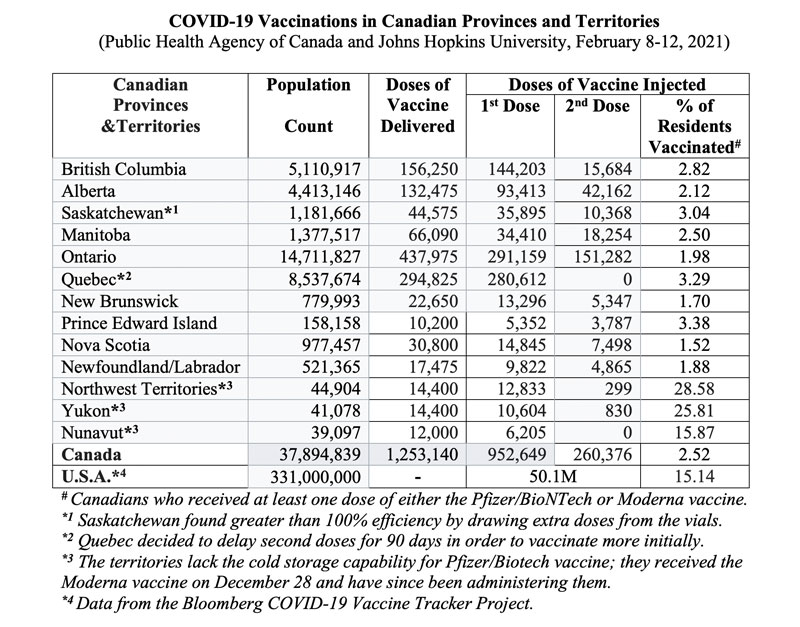
The Northwest Territories and the Yukon have over a fourth (28.58% and 25.81%, respectively) of their citizens already vaccinated, notwithstanding they started much later than the provinces. Nunavut came in third place at 15.87%. The provinces range in their inoculation rates from 1.52% (Nova Scotia) to 3.38% (Prince Edward Island).
Path to Population (‘Herd’) Immunity
It is generally accepted that vaccinating 70% to 85% of a country’s population would enable a return to normalcy. Dr. Anthony Fauci, an acknowledged world expert on pandemics, has reiterated this teaching reminder often.
The concept is known as ‘herd’, community or population immunity. As more people get vaccinated, they start to build a group that builds a collective defence against the virus so that isolated occurrences of infection burn out instead of spreading unchecked into an outbreak. Herd immunity is achieved when enough people are protected that it begins to have a measurable effect on the speed of transmission and could even begin well before 75% of the population are fully vaccinated. Or, it is the point when outbreaks can no longer be sustained to ripple across the country and beyond national boundaries.
Today in the U.S. the latest vaccination rate averages 1,656,452 doses daily. At this rate, it will take about 8 months to cover 75% of their population with a two-dose vaccine.
In contrast, Canada has administered a total of 1,213,025 doses over a period of 68 days from December 14, 2020 when the first Canadian patient received her jab, effectively yielding an average of 17,838 doses daily during this interval period. Based on this initial experience, “Can Canada vaccinate all her residents against COVID-19 by December 31, 2021?”
Let us do the arithmetic:
- We have vaccinated 52% of the 37,894,939 Canadian population (see Table above), that is, 954,952 residents. [ 37,894,939 X 2.52% = 954,952 vaccinated Canadians]
- Thus, we need to vaccinate the remaining 36,939,987 non-vaccinated population. [37,894,939 - 954,952 = 36,939,987 non-vaccinated Canadians]
- If we vaccinate at least 75% of these yet non-vaccinated to attain population or ‘herd’ immunity, we need to vaccinate at least 27,704,990 [36,939,987 X 75% = 27,704,990 Canadian residents]
- Since two doses are required for full vaccine efficacy, we need to do 55,409,980 injections to 27,704,990 residents to reach the minimum numbers that create ‘herd’ immunity. [27,704,990 X 2 = 55,409,980 injection doses]
- We would need to do 181,078 injections daily for 306 days non-stop until December 31, 2021 to succeed in vaccinating the needed minimum numbers of Canadians to reach the minimum number required for the attainment of population immunity and for individual protection. [55,409,980/306 = 181,078 injections doses daily]
- If we overlook and unwittingly continue with our current pace of 17,838 injection doses daily, we are alarmingly looking at 8 ½ years ahead of us to reach our universal goal.
[55,409,980/17,838 = 3,106 days; 3,106/365 = 8.5 years]- This might serve as a wake-up call to public health officials and political leaders;
- With the temporary disruptions being solved soon and vaccine supply being resumed, we could expect a rebound and vaccination rates could be expected to climb.
- And Canada has made more contracts to purchase more vaccines, not to mention to establish our manufacturing firm inland.
- Nonetheless, it is well to remember that until then we will need to do 181,078 injection doses daily NON-STOP, WEEKENDS INCLUDED, until December 31, 2021 to reach our vaccination goal before the New Year Eve 2022 strikes the clock.
Note Well: The answer is obvious. We have to move now, plan and put the resources of the nation – led by our Prime Minister and the Premiers of provinces and Leaders of Territorial governments to act in unison with our public health officials and experts. We need the supplies of vaccines and needles and alcohol swabs, uninterrupted; the personnel and budget required; the vaccination sites identified and accessible; volunteer health corps contacted; the health care corps of the Reserve and Armed Forces, if need be, mobilized; and clear lines of command and action defined.
In fact, Lauren Pelley of CBC News posted on February 06 “What Canada could do to take advantage of the lull in COVID-19 vaccine shipments” and listed the following points she had gathered from the community:
- build up community outreach,
- decentralize vaccination sites,
- combat vaccine hesitancy,
- address education, and
- provide information for our communities, especially new immigrants and refugees
I would add governments should continue to engage more community media outlets, both print and online.
Pfizer Vaccine Supply to Resume
It is good news, as reported by Mia Rabson of the Canadian Press (Feb 11), that “Canada’s vaccine deliveries set to more than quadruple next week with largest Pfizer shipment yet.” There is a spoiler: Moderna’s next shipment on February 22 will now be “only two-thirds of what it was supposed to be.”
“Pfizer will need to ship 450,000 doses a week on average in the last two weeks of March to meet its contract for four million doses by March 31. Moderna will need to ship about 1.3 million doses in March to meet its contract to ship two million doses by the same date.”
Maj.-Gen. Dany Fortin, who oversees Canada’s vaccine distribution, says “Pfizer has confirmed it will ship 403,000 does next week, 475,000 the week after that, and then 444,000 doses in each of the first two weeks of March.”
The recent disruptions in supply underscore the need for a vaccine manufacturing plant in Canada.
Vaccination Alone a Vital Step, but Not Enough to End Pandemic
Questions continue to be asked even as we pursue our mass vaccination drive. Let me do half-a-dozen Question & Answer summary here of what vaccine scientists and public health experts have taught us to help us better understand about the virus behaviour and the human host response, even as research scientists search for definitive answers and public health experts and frontline health care workers share their insights from learned field and clinical experience and I paraphrase and quote:
Q1. Why should I continue with the usual pandemic precautions – avoiding crowds, continuing to wear a good mask in public, maintaining 6 feet or more of distance from people outside your household and frequently washing your hands – after getting the COVID-19 vaccine?
A1. The answer is to protect yourself – the vaccine recipient – at least for a while. Vaccine's effectiveness takes time to build up, that is, not to get sick with COVID-19 following vaccination. With the Pfizer-BioNTech vaccine, protection does not start until 12 days after the first shot and that it reaches 52% effectiveness a few weeks later. A week after the second vaccination, the effectiveness rate hits 95%.
With the Moderna vaccine, the protection rate is 51% two weeks after the first dose and 94% two weeks after the second dose.
That is not 100% for both vaccines. This means one out of every 20 people who get either vaccine could still get moderate to severe infection. Moreover, we are presently seeing new infections from new variants of the virus and scientists are closely monitoring the developments.
Q2. Can I spread the virus to others even if I am fully vaccinated with the two doses?
A2. Vaccine scientists studying the effectiveness of the vaccine shots do not have an answer yet. The data are just now being collected. The government regulators, before approving the Moderna and Pfizer vaccines, asked the vaccine manufacturers only whether their products protect people from COVID-19 symptoms. They did not ask if the vaccines stop people who have been vaccinated from nevertheless spreading the virus to others. The emergency authorizations that have allowed distribution of the two new vaccines cite only their ability to keep you — the person vaccinated — from becoming severely sick with COVID-19.Public health experts advise the answer is ‘yes’ until we get the needed scientific data and knowledge.
Q3. How can one spread a virus if he or she has been vaccinated?
A3. The COVID-19 vaccines rely on bits of genetic material or virus protein — not anything that could grow into an active SARS-CoV-2 virus which causes the disease COVID-19. The concern instead with the vaccine is about whether one might still have an asymptomatic infection despite immunization – meaning, without symptoms and signs of the disease – but still able to shed the virus.
To further explain, imagine you have been vaccinated and you encounter SARS-CoV-2. You are much less likely to develop symptoms, but your immune system may not fight off the virus completely. Thus, some viruses may survive, reproduce in the body, and get expelled from your nose or mouth in a breath, cough, sneeze, shout or song. No one can be sure yet if this actually happens or if it happens often enough that you would be emitting enough active virus to sicken someone else. This is our current state of knowledge.
Q4. Why did the government regulators not demand information on infectivity before authorizing the first two vaccines?
A4. “In a word, time,” said Dr. Larry Corey, a virologist at the Fred Hutchinson Cancer Research Center at the University of Washington in Seattle who leads the COVID-19 Prevention Network (a U.S. federally funded consortium of vaccine experts who have been testing vaccines). "We wanted to get an answer quickly," Dr. Corey said, and to do so required as simple an experimental protocol as possible. He added: “Each of the 75,000 volunteers for the clinical trials of the Pfizer and Moderna vaccines had to come into a clinic; get a test for the coronavirus; get either a vaccine or a placebo shot (without knowing which they have received); return for a second shot; and come back to the clinic for testing anytime in the interim if they showed any symptoms of having caught the virus. Adding in even more coronavirus tests along the way to see if the vaccinated volunteers had picked up or were transmitting the virus (which would have provided the definitive answers to the questions asked) would have delayed the initial results considerably. And in the midst of the (deadly) pandemic, speed was of the essence.”
Q5. Now that I am vaccinated, can I take my mask off in a crowded room if everyone else has also been vaccinated?
A5. Not quite yet. Remember that the two vaccines are not 100% effective, and many in the research community still advise caution. Once most people are protected and there is less virus circulating in the air — and less circulating in the community — the advice and restrictions on this may ease up a bit. Crowd avoidance and hand-washing will help stop the spread.
Q6. What is the bottom line?
A6. With the magnitude of cases and deaths still around as shown in the Table at the beginning of this Commentary, intensive care and emergency room specialists and nurses and other health care workers in the hospital who attend first-hand to COVID-19 patients really want you to continue to wear a mask, keep your distance and wash your hands, even if you've been vaccinated – until the research on shedding has yielded some answers. My advice is the same advice I give to myself and family: Continue with the other advisory public health measures, and especially wear a mask (look for the newest high-quality masks) until vaccine scientists have the data. More so now that new variants of the virus have been reported in all Canadian provinces. Vaccination alone is a vital step to stop the pandemic, but not enough; heed the needed public health precautions.